We will bill your insurance given we have been provided the information on a timely basis. If we are contracted with your insurance, you will be sent a statement after we receive an Explanation of Payment/Benefits. If we are not contracted, understand that only you have a relationship with that payer. We will give your insurance 45 days to pay. If they do not pay within 45 days, you will be held responsible.
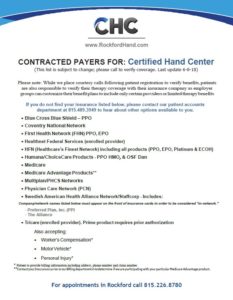
Contracted Insurance Providers
Proud Providers of The Zero Card
Your First Visit
We understand that paperwork is a nuisance for all; however, because we are a privately owned clinic not directly associated with any specific physician practices, you will need to provide certain information directly to us. Please refer to the Patient Forms tab for the proper forms and information you will need to bring to your first appointment. It is your responsibility to give us the correct billing information at your first visit. If we are given information at a later date that is to be retroactive, we cannot guarantee that we will be able to accommodate your request, but we will make every effort within reason. If you have some form of insurance/coverage, we would prefer to collect from them versus you as a patient!
Because we strive to get patients in as quickly as possible, we will gather the billing information at your initial visit. We encourage you to contact your insurance directly to determine your physical therapy benefits and if authorization is required. The responsibility for the authorization process varies depending on the insurance company/benefit plan and can often be the patient, referring physician or our responsibility so you will want to understand this. Authorizations can be a source of problems. If we are aware that an authorization is needed and we do not have one on file, you will be given the option to continue care at your own expense potentially or postpone treatment until authorization can be obtained. If you are told by your insurance conflicting information about our status as a contracted provider, please contact our Patient Accounts so we can make sure our information is listed correctly with the insurance companies.
We will be in contact with your primary insurance to verify eligibility, therapy benefits and if authorization is required for our services. We do not contact secondary or tertiary insurances unless your coverage with them is an HMO. As you are probably aware, insurance companies make it very clear when you or a provider calls to verify benefits that the information provided during these calls is “not a guarantee of benefits or payment” until the claims are received and processed. We will make every effort to inform you of limited benefits or when benefits are about to terminate; however, you are ultimately responsible so please don’t hesitate to ask about the status of your benefits by calling our Patient Accounts or your insurance company directly. Please note: We will only be able to give an estimate; the final amounts can only be determined once claims are billed and processed. If you have a copay for therapy services, this is due at the time of service.